724
Views & Citations10
Likes & Shares
Helicobacter pylori are the most prevalent chronic
bacterial infection. It is associated with peptic ulcer disease, chronic
gastritis, gastric adenocarcinoma and gastric Mucosa Associated Lymphoid
Disease (MALT) lymphoma. HpSA Enzyme Immunoassay (EIA) is an in vitro qualitative procedure for the
detection of Helicobacter pylori
antigens in human stool. Test results are intended to aid in the diagnosis of H. pylori infection and to monitor
response during and post therapy in patients.
Keywords: HpSA, Endoscopy, PPI, UBT
INTRODUCTION
Helicobacter pylori are the most prevalent chronic
bacterial infection and are associated with peptic ulcer disease, chronic
gastritis, gastric adenocarcinoma and gastric Mucosa Associated Lymphoid Tissue
(MALT) lymphoma [1,2]. It is a Gram-negative, microaerophilic bacterium usually
found in the stomach. The Australian scientists Barry Marshall and Robin Warren
found it in the stomach of a person in 1982 with chronic gastritis and gastric
ulcers. It was not previously believed to have a microbial cause [3]. It is
also linked to the development of duodenal ulcers and stomach cancer [4].
However, over 80% of individuals infected with the bacterium are asymptomatic.
In recognition of their discovery, Marshall and Warren were awarded the 2005
Nobel Prize in Physiology or Medicine. Upto 90% of people infected with H. pylori never experience symptoms [5].
Acute infection may appear as an acute gastritis with abdominal pain or nausea.
This develops into chronic gastritis and non-ulcer dyspepsia: stomach pains,
nausea, bloating, belching and sometimes vomiting or black stool [6].
CASE REPORT
A 65 year old female was suffering from acid
peptic disease with epigastric pain since last 20 years. She was treated with
proton-pump inhibitors such as omeprazole. She was afraid of taking any spicy
or non-vegetarian food which increased the symptoms. She was not tolerating
citrus fruits and milk products except curd. She was a non-diabetic and
moderately hypertensive. Ultrasound scanning of whole abdomen was done. No
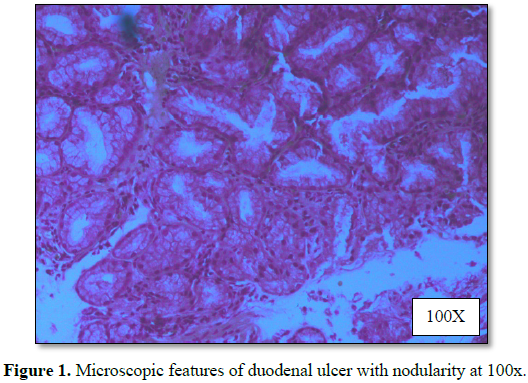
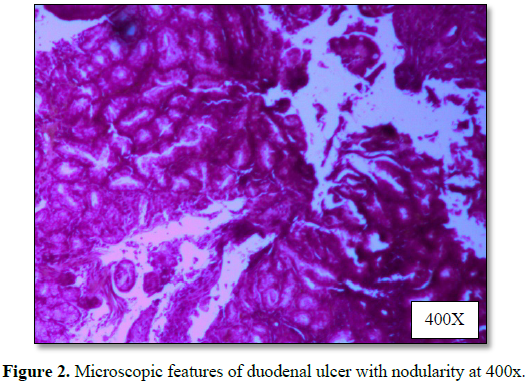
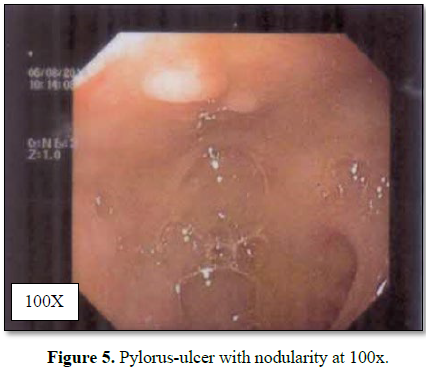
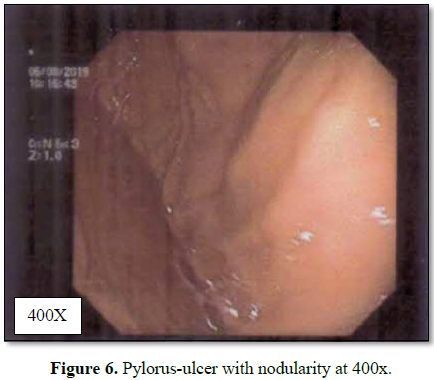
significant abnormality was detected. Upper GI endoscopy suggested mucosal
hyperemia with erosions in the antrum and multiple tiny superficial ulcers with
nodularity over anterior and superficial wall in the first part of duodenum.
The rapid urease test was found positive. Enzyme immunoassay for the detection
of monoclonal antigens of Helicobacter
pylori in stool found positive in high titer. Two courses of triple drug
therapy were given at two weeks interval. The HpSA test became negative.
DISCUSSION
Helicobacter pylori is now recognized as one of the
most common and medically important pathogen worldwide [7]. The diagnostic test
for H. pylori can be categorized as
invasive (endoscopy, biopsy, culture) or non-invasive (stool antigen test,
carbon urea breath test and blood antibody tests). An endoscopic biopsy is an
invasive means to test H. pylori
infection. Low level of infection can be missed by biopsy. So multiple samples
are recommended. The most accurate method for detecting the bacteria is with
histological examination from two sites after endoscopy biopsy, combined with
either a rapid urease test or microbial culture [8].
An endoscopy biopsy is an invasive means to
test for H. pylori infection.
Low-level infections can be missed by biopsy, so multiple samples are recommended.
The most accurate method for detecting H.
pylori infection is histological examination from two sites combined with
rapid urease test [10].
Urea breath testing is based upon the
hydrolysis of urea by H. pylori to
produce CO2 and ammonia. Urea with a labeled carbon isotope is given
by mouth. The liberated CO2 is detected in breath samples. The tests
can be performed in 15-20 min and have similar cost and accuracy. This method
is not preferred in young children and pregnant women though the dose of
radiation is small [11,12].
Stool antigen assay detect H. pylori infection. The monoclonal
enzyme immunoassay is highly sensitive (94-97%). Stool antigen testing can
therefore be used to establish the initial diagnosis of H. pylori and to confirm eradication [13,14].
Among all the available tests, stool antigen testing is the most cost-effective
in areas of low to intermediate prevalence of H. pylori. This test is predictive of eradication as early as seven
days after completion of therapy. False negative results can be avoided by stop
taking antibiotics for four weeks and PPIs for one to two weeks prior to
testing (Table 1 and Figures 1-7).
CONCLUSION
Endoscopy is not indicated solely for the
purpose of establishing H. pylori
status. Stool antigen test is the choice of test for diagnosis and eradication
of the bacteria .It is the most cost effective test in areas of low to
intermediate prevalence of H. pylori.
1. Chang AH, Parsonnet J (2010) Role of bacteria in
oncogenesis. Clin Microbiol Rev 23: 837-857.
2. Center for Disease Control (2017) Helicobacter
pylori. Available at: http://www.cdc.gov
3. (2018) The Nobel prize in physiology or medicine
2005.
4. Amieva M, Peek RM (2016) Pathobiology of Helicobacter
pylori - Induced gastric cancer. Gastroenterology 150: 64-78.
5. Bytzer P, Dahlerup JF, Eriksen JR, Jarbøl DE,
Rosenstock S, et al. (2011) Diagnosis and treatment of Helicobacter pylori
infection. Dan Med Bull 58: C4271.
6. Wang YK, Kuo FC, Liu CJ, Wu MC, Shih HY, et al.
(2015) Diagnosis of Helicobacter pylori infection: Current options and
developments. World J Gastroenterol 21: 11221-11235.
7. Granstrom M, Lehours P, Bengtsson C, Mégraud F
(2008) Diagnosis of Helicobacter pylori. Helicobacter 13: 7-12.
8. Ricci C, Holton J, Vaira D (2007) Diagnosis of Helicobacter
pylori: Invasive and non-invasive tests. Best Pract Res Clin Gastroenterol
21: 299-313.
9. Monteiro L, de Mascarel A, Sarrasqueta AM, Bergey
B, Barberis C, et al. (2001) Diagnosis of Helicobacter pylori infection:
Non-invasive methods compared to invasive methods and evaluation of two new
tests. Am J Gastroenterol 96: 353-358.
10. Megraud F, Lehours P (2007) Helicobacter pylori
detection and antimicrobial susceptibility testing. Clin Microbiol Rev 20: 280.
11. Atherton JC, Spiller RC (1994) The urea breath test
for Helicobacter pylori. Gut 35: 723-725.
12. Perri F, Manes G, Neri M, Vaira D, Nardone G (2002)
Helicobacter pylori antigen stool test and 13C-urea breathe test in
patients after eradication treatments. Am J Gastroenterol 97: 2756-2762.
13. Shimoyama T (2013) Stool antigen tests for the
management of Helicobacter pylori infection. World J Gastroenterol 19:
8188-8191.
14. Gisbert JP, De La Morena F, Abraira V (2006) Accuracy
of monoclonal stool antigen test for the diagnosis of H. pylori
infection: A systematic review and meta-analysis. Am J Gastroenterol 101:
1921-1930.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Advance Research on Endocrinology and Metabolism (ISSN: 2689-8209)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- BioMed Research Journal (ISSN:2578-8892)
- Journal of Infectious Diseases and Research (ISSN: 2688-6537)
- Journal of Cancer Science and Treatment (ISSN:2641-7472)
- Journal of Neurosurgery Imaging and Techniques (ISSN:2473-1943)
- Journal of Otolaryngology and Neurotology Research(ISSN:2641-6956)